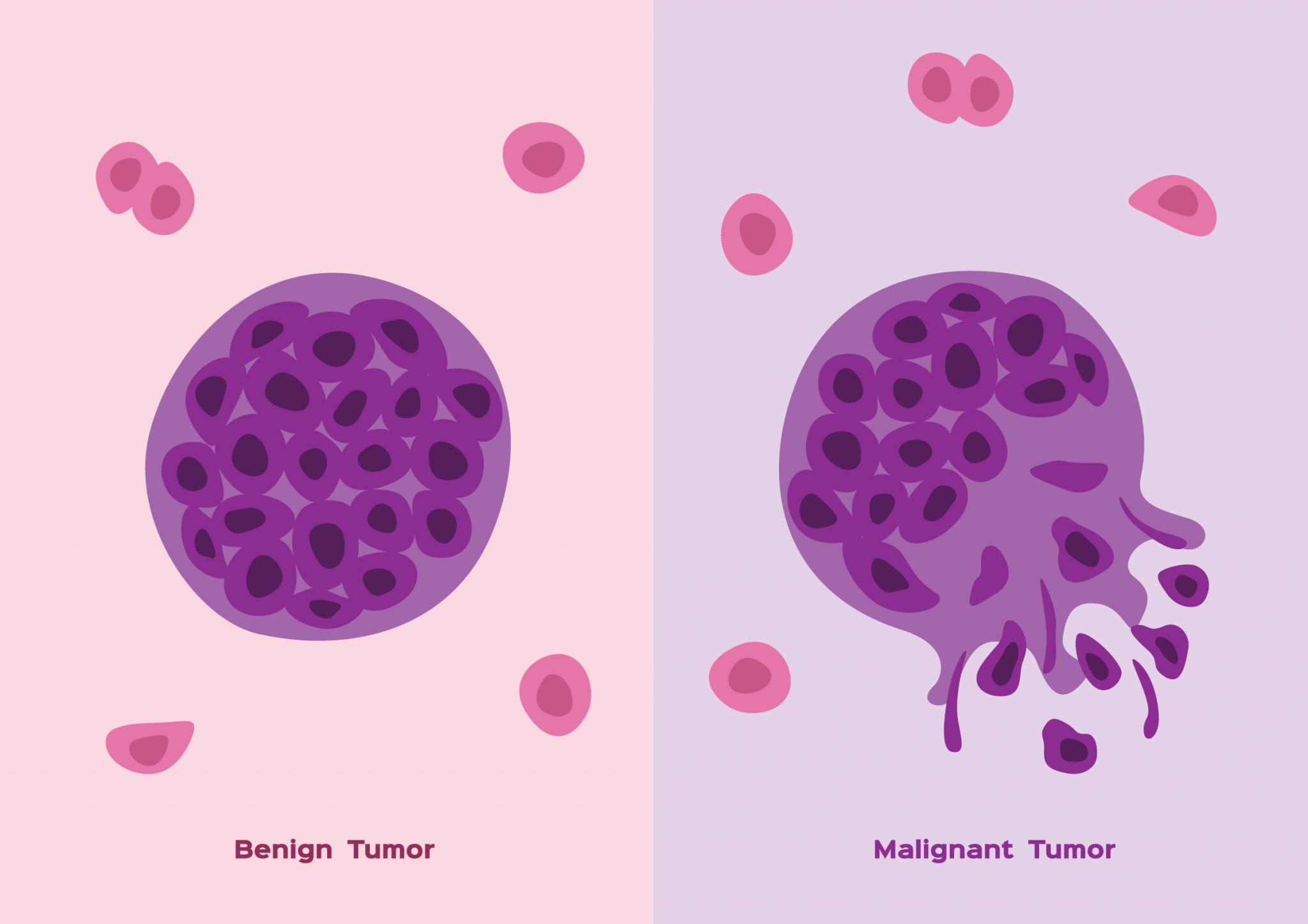
Tumors are abnormal masses caused by excessive or uncontrolled cell division. These tumors can form in nearly every organ or tissue, including the brain, liver, bones, and soft tissues. The way they grow, spread, or affect the body varies depending on their classification. That distinction matters significantly when discussing patient outcomes. Some tumors may stay silent for years, while others invade surrounding structures within weeks. Understanding their behavior is key to determining the treatment plan and long-term follow-up. Not every mass you feel under your skin is cause for alarm, but some demand immediate attention.
Their boundaries are often well-defined and encapsulated
Benign tumors tend to grow slowly. Their boundaries are often well-defined and encapsulated. That means the cells usually remain in one place and do not spread to other organs. Surgeons often remove benign tumors with clear margins because they are less invasive. The fibrous capsule surrounding many benign tumors keeps the mass separated from nearby tissue. This makes surgical removal safer and reduces the chance of recurrence. Benign tumors can still cause trouble if they press on a nerve, artery, or duct. But they are not considered life-threatening unless they interfere with vital functions.
Unlike benign tumors, malignant ones often invade surrounding tissue
Unlike benign tumors, malignant ones often invade surrounding tissue. This invasion can make them difficult to remove completely. Malignant cells may lose their structure, grow irregularly, and form projections into nearby organs. The edges of malignant tumors are typically ragged, without a distinct border. As they invade, they destroy normal cells and disrupt organ function. This infiltrative nature is one of the reasons why early detection is critical. Even a small malignant tumor can spread rapidly, depending on its type and location.
Metastasis involves tumor cells entering blood or lymphatic vessels
One of the defining features of malignant tumors is their ability to metastasize. Metastasis involves tumor cells entering blood or lymphatic vessels, traveling to distant parts of the body. Once they arrive, they may form new tumors in other organs. For example, lung cancer may spread to the brain or bones. Breast cancer often moves to the liver or lungs. These secondary tumors may not resemble the original tissue type. That’s why oncologists usually treat metastatic tumors based on their primary origin, not their new location. The presence of metastasis usually changes the stage and prognosis dramatically.
They can resemble the tissue they come from
Benign tumors often look similar to the tissue they come from. They may even retain some normal functions. For instance, a benign thyroid nodule might still produce hormones. A lipoma will resemble fat tissue and feel soft to the touch. Pathologists recognize these traits when examining samples under a microscope. Malignant tumors, however, usually lose that resemblance. The more abnormal the cells look, the more aggressive the tumor tends to be. These cellular changes include larger nuclei, frequent mitoses, and irregular arrangements. The term “differentiation” describes how closely tumor cells resemble normal ones. Poor differentiation often signals a worse outcome.
Some grow so slowly that people live with them for decades
Some benign tumors grow so slowly that people live with them for decades. A person may discover a lump in their arm or neck that hasn’t changed in years. In many cases, no intervention is needed unless the tumor causes discomfort or dysfunction. Doctors might monitor these tumors with periodic imaging or physical exams. Malignant tumors don’t usually allow for such patience. Their fast growth and unpredictable behavior require quicker decisions. In some rare cases, a slow-growing malignancy may be confused with a benign mass until biopsy results reveal the truth.
Biopsy remains the most reliable method for diagnosis
Imaging tests may suggest whether a tumor is likely benign or malignant, but they aren’t definitive. Biopsy remains the most reliable method for diagnosis. A tissue sample allows doctors to examine cellular structure and behavior directly. Sometimes fine-needle aspiration is enough. Other times, a core needle or surgical sample is required. The pathologist looks for patterns like mitotic activity, necrosis, and nuclear changes. These details reveal the tumor’s nature and help determine next steps. Radiologists and oncologists often work together to interpret both imaging and pathology results to reach a clear diagnosis.
Symptoms depend on size, location, and pressure effects
Symptoms of a tumor don’t always reflect its danger level. Symptoms depend on size, location, and pressure effects. A benign tumor in the brain can cause seizures if it presses against certain regions. A malignant one in the skin might go unnoticed until it metastasizes. Some tumors bleed internally or obstruct organs. Others cause pain, weight loss, or hormonal changes. Hormone-producing tumors, even if benign, may create significant metabolic issues. That’s why a full evaluation includes imaging, lab tests, and a review of medical history.
Tumor markers in blood are sometimes useful but not always specific
Doctors may also check blood for tumor markers, which are substances released by certain cancers. Tumor markers in blood are sometimes useful but not always specific. Elevated PSA might suggest prostate cancer. High CA-125 levels could indicate ovarian tumors. But these markers also rise in non-cancerous conditions. Their primary role is often in monitoring treatment or checking for recurrence. They rarely provide a definitive diagnosis on their own. So, while helpful, they’re just one piece of a much larger diagnostic puzzle.
Treatments vary depending on type, location, and behavior
Not all tumors require treatment. Treatments vary depending on type, location, and behavior. Benign ones may be left alone, especially if small and stable. Some require surgery due to pain, obstruction, or cosmetic concerns. Malignant tumors almost always need intervention. This may include surgery, chemotherapy, radiation, immunotherapy, or targeted drugs. Sometimes multiple treatments are combined for better outcomes. Treatment decisions also consider patient age, overall health, and personal preferences. Even the same type of tumor may require a different approach in two people.
Margins of excised tumors tell surgeons if any cells were left behind
After surgery, pathologists check the margins of excised tumors. Margins of excised tumors tell surgeons if any cells were left behind. A “clean margin” means no tumor cells at the edge, suggesting complete removal. A “positive margin” indicates residual disease, which may require more treatment. In malignant tumors, even microscopic cells left behind can regrow or spread. Some cancers, like melanoma, need wide margins to prevent recurrence. That’s why pathology reports often include detailed notes about margins, size, and invasion depth.
Even benign tumors can complicate pregnancy or organ development
In specific contexts, even benign tumors can pose serious risks. Even benign tumors can complicate pregnancy or organ development. A fibroid in the uterus may interfere with fertility or delivery. A brain cyst can block fluid flow and increase pressure. Pediatric tumors may alter bone growth or hormone regulation. So, being non-cancerous doesn’t mean being harmless. Location, timing, and underlying conditions all affect how a tumor behaves and what intervention it needs.
Some tumors arise from genetic mutations inherited across generations
Tumors don’t appear randomly. Some tumors arise from genetic mutations inherited across generations. Others result from environmental exposures or random cell errors. Certain cancers run in families, such as those linked to BRCA genes. Genetic counseling may help families understand their risks and plan screenings. Benign tumors also have hereditary patterns, like neurofibromatosis or familial adenomatous polyposis. Identifying these patterns early can guide preventive care. Genetics plays a large role, but lifestyle factors also matter—smoking, alcohol, radiation, or infections all contribute.
Recurrent tumors may behave differently from the original
Sometimes a tumor returns even after treatment. Recurrent tumors may behave differently from the original. They may grow faster, become resistant to drugs, or spread more aggressively. Follow-up care often involves regular imaging, lab tests, and clinical exams. Patients with high-risk tumors need tighter surveillance schedules. Even those with benign tumors may face recurrence if removal was incomplete. A recurrence doesn’t always mean poor prognosis, but it usually demands a revised treatment plan.
The absence of spread is not always a guarantee of safety
Early stages of tumor growth can be deceiving. The absence of spread is not always a guarantee of safety. Some malignant tumors remain localized for a long time before they metastasize. Others may have already spread microscopically by the time they are found. That’s why staging includes not only tumor size but lymph node involvement and distant spread. Staging guides therapy and gives patients a clearer picture of their condition. Doctors often use systems like TNM or grade scales for consistency.
Source: Best Oncologist in Dubai / Best Oncologist in Abu Dhabi