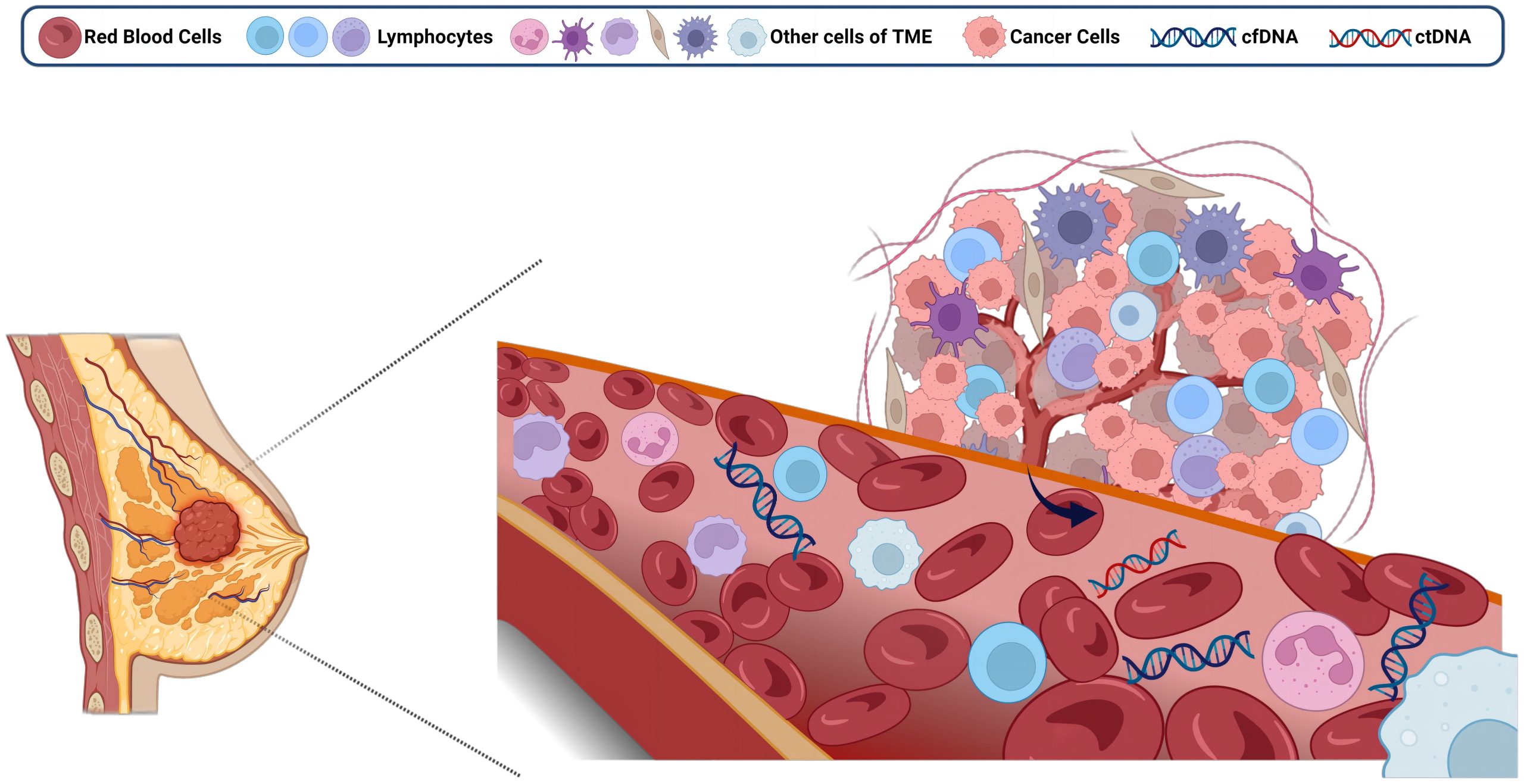
In the complex world of health, certain clues help doctors. Tumor markers are one such clue. They are substances found in the body. Cancer cells, or other cells, produce them. Sometimes, non-cancerous conditions also cause them. They can be found in blood or urine. Doctors use them in various ways. They aid in cancer detection. They help monitor treatment effectiveness. Understanding them is very important.
Tumor markers are one such clue.
Think of tumor markers as signals. They are molecules linked to cancer. They can be proteins or enzymes. Hormones or other substances too. These are produced in excess. This happens due to cancer growth. Sometimes, normal cells react to cancer. They produce these markers as well. The presence of a marker is a hint. It suggests something is happening.
Cancer cells, or other cells, produce them.
The origin of markers varies. Cancer cells themselves can create them. This often happens during rapid growth. Other times, normal cells respond. They produce markers in cancer’s presence. This indicates the body’s reaction. It’s a complex biological interplay. The source helps doctors interpret. It gives insight into the process. This distinction is subtle.
They can be found in blood or urine.
Doctors collect samples for testing. Blood tests are the most common. A simple blood draw is usually enough. Urine samples can also be used. Less often, tissue samples are tested. This makes monitoring relatively easy. It’s not overly invasive for patients. The sample collection is straightforward. Results provide valuable information.
Doctors use them in various ways.
Tumor markers have several roles. They help in cancer detection. They aid in staging the disease. They guide treatment choices often. They monitor how well treatment works. They can detect cancer recurrence. No single marker works for all cancers. A panel of markers is often used. This comprehensive view helps decisions.
They aid in cancer detection.
Tumor markers are rarely diagnostic alone. They’re not a definitive cancer test. High levels suggest a need for more tests. Imaging, biopsies confirm diagnosis. Markers alert doctors to possibilities. They help identify high-risk individuals. They can signal early changes. This early warning is very helpful. It prompts timely investigation.
They help monitor treatment effectiveness.
This is a key application. Falling marker levels often mean treatment works. Rising levels might signal progression. This allows doctors to adjust therapy. They can switch medications. They can change treatment plans. It provides real-time feedback. This monitoring is invaluable. It optimizes patient care continuously. It helps manage expectations.
Understanding them is very important.
Knowing what markers mean empowers you. High levels don’t always mean cancer. Many non-cancerous conditions raise them. Inflammation, infection, even benign tumors do. Low levels don’t rule out cancer. It’s a piece of the puzzle. Discuss results thoroughly with your doctor. Avoid self-diagnosis always. Interpretation needs medical expertise.
Many non-cancerous conditions raise them.
This point is crucial for patients. Inflammation can elevate markers. Liver disease might cause a rise. Kidney problems can also affect levels. Pregnancy can impact some markers. Certain medications might interfere. This wide range of causes exists. It means careful interpretation is vital. A high result is just a signal. It necessitates further investigation.
Low levels don’t rule out cancer.
A normal marker result doesn’t mean safety. Some cancers don’t produce markers. Or they produce them in low amounts. Very early cancers might not show up. Marker levels can fluctuate too. They are not foolproof indicators. Doctors combine marker tests. They use them with other diagnostic tools. Clinical context is always paramount.
Discussion results thoroughly with your doctor.
Never interpret results alone. Your doctor understands your full picture. They know your medical history. They consider all your symptoms. They weigh marker levels against other tests. They explain what each number means. They discuss next steps clearly. Ask all your questions openly. This dialogue is essential. It ensures proper understanding.
Common Tumor Markers Explained
Different cancers have specific markers. Prostate-Specific Antigen (PSA) for prostate cancer. Carcinoembryonic Antigen (CEA) for colon cancer. CA-125 for ovarian cancer. Alpha-Fetoprotein (AFP) for liver/testicular. CA 19-9 for pancreatic cancer. Beta-human chorionic gonadotropin (hCG) for germ cell. Each has its own nuances.
Prostate-Specific Antigen (PSA) for prostate cancer.
PSA is a common blood test. It helps screen for prostate cancer. High PSA can indicate cancer. But it also rises with benign prostate enlargement. Infection can elevate it too. It’s used for monitoring treatment. Post-treatment, falling PSA is good. Rising PSA might mean recurrence. It’s a useful tracking tool.
Carcinoembryonic Antigen (CEA) for colon cancer.
CEA is another well-known marker. It’s often used for colon cancer. Also seen in lung, breast, stomach cancers. It’s not for screening the general population. It helps monitor known cancer. After surgery, if CEA falls, it’s positive. If it rises, recurrence might be suspected. It reflects disease activity effectively.
CA-125 for ovarian cancer.
CA-125 is mainly for ovarian cancer. It helps monitor treatment response. High levels often mean ovarian cancer. But it also rises with endometriosis. Or pelvic inflammatory disease. It’s not a screening test for everyone. It’s most valuable in known cases. It guides therapy adjustments. It helps predict prognosis sometimes.
Alpha-Fetoprotein (AFP) for liver/testicular.
AFP is linked to specific cancers. It’s a marker for liver cancer. Also for testicular and ovarian germ cell tumors. It’s useful in diagnosis of these. It helps track treatment success. High levels often indicate disease. Falling levels suggest response. It’s also used in prenatal screening. This is a different application.
CA 19-9 for pancreatic cancer.
CA 19-9 is used for pancreatic cancer. It also rises in bile duct cancer. It’s not suitable for general screening. Many benign conditions can elevate it. It helps monitor treatment effectiveness. It aids in assessing disease progression. High levels often indicate advanced disease. It’s a challenging marker to interpret.
Beta-human chorionic gonadotropin (hCG) for germ cell.
hCG is known as a pregnancy hormone. But it’s also a tumor marker. It’s used for germ cell tumors. These occur in testes or ovaries. It’s very useful for monitoring. High levels suggest tumor presence. Falling levels show treatment success. It’s a sensitive indicator for these cancers.
New markers are always emerging.
Research constantly progresses. Scientists discover new biomarkers. These new markers offer more specificity. They can improve diagnostic accuracy. They might allow for earlier detection. Personalized medicine relies on them. This field is rapidly advancing. Future cancer care will benefit. Stay informed about developments.
This field is rapidly advancing.
Genomic testing is expanding. Understanding cancer at a molecular level. This allows for targeted therapies. Tumor markers fit into this picture. They provide insights into biology. Research identifies new proteins. Technology allows better detection methods. This progress offers new hope. It reshapes cancer management.
Tumor markers are substances, often found in blood, that can indicate cancer presence or progression, aiding in monitoring treatment and recurrence, but require careful medical interpretation.